Prostatitis is an inflammatory disease of the prostate gland. It is manifested by frequent campaigns in the toilet, pain in the penis, scrotum, rectum, sexual disorders (erection, early ejaculation, etc. ), sometimes delayed urine, and blood insurance in urine. The diagnosis of prostatitis is established by a urologist or other specialist in a typical clinical picture, the results of a rectal study. Additionally, an ultrasound of the prostate, sowing bacteria of prostatic secretion and urine are carried out. Conservative treatment - antibacterial therapy, immunotherapy, prostate massage, lifestyle correction.
General information
Prostatitis - inflammation of the seed (prostate) gland - prostate. It is the most common disease of the genitourinary system in men. Most often it affects patients aged 25-50 years. In accordance with various data, prostatitis suffers from 30-85% of men over the age of 30. Perhaps abscessing the prostate gland, inflammation of the testicles and appendages, which threatens infertility. The ascent of the infection leads to inflammation of the upper parts of the genitourinary system (cystitis, pyelonephritis).
Pathology develops when an infectious agent is entered, which enters the prostate fabric from the organs of the genitourinary system (urethra, bladder) or from remote inflammatory focus (with pneumonia, flu, tonsillitis, furunculosis).
The causes of prostatitis
A golden staphylococcus aureus (Enterococcus), Enterobacter (Enterobacter), Pseudomonas (Pseudomonas), Proteus (Proteus), and Klebcelllah, and Klebcelllah can act as an infectious agent in an acute process. (Klebsiella) and E. coli (E. coli). Most microorganisms belong to the conditionally pathogenic flora and causes prostatitis only if there are other predisposing factors. Chronic inflammation is usually caused by Paul with microbial associations.
The risk of developing the disease increases during hypothermia, the presence of specific infections and conditions in the history of congestion in the tissues of the prostate. The following predisposing factors are distinguished:
- General hypothermia (single or permanent, related to working conditions).
- A sedentary lifestyle, a specialty forcing a person to be in a sitting position for a long time (computer operator, driver, etc. ).
- Constant constipation.
- Violations of the normal rhythm of sexual activity (excessive sexual activity, prolonged abstinence, incomplete ejaculation during the deprived of the emotional coloring of the "usual" sexual intercourse).
- The presence of chronic diseases (cholecystitis, bronchitis) or chronic infectious foci in the body (chronic osteomyelitis, absurd caries, tonsillitis, etc. ).
- Transferred urological diseases (urethritis, cystitis, etc. ) and sexually transmitted diseases (trichomoniasis, gonorrhea).
- States that cause inhibition of the immune system (chronic stresses, irregular and inferior nutrition, regular lack of sleep, a state of overtraining in athletes).
It is assumed that the risk of developing pathology increases with chronic intoxications (alcohol, nicotine, morphine). Some studies in the field of modern andrology prove that the provoking factor is a chronic crotch injury (vibration, concussion) in motorists, motorcyclists and cyclists. However, the overwhelming number of experts believes that all of the listed circumstances are not real causes of the disease, but only contribute to the exacerbation of the latent inflammatory process in the tissues of the prostate.
The decisive role in the occurrence of prostatitis is played by stagnation in the tissues of the prostate. Violation of capillary blood flow causes an increase in lipid peroxidation, edema, exudation of prostate tissues and forms conditions for the development of the infectious process.

Symptoms of prostatitis
Acute prostatitis
There are three stages of acute prostatitis, which are characterized by the presence of a certain clinical picture and morphological changes:
- Sharp catarrhal. Patients complain of rapid, often painful urination, pain in the sacrum and perineum.
- Sharp follicular. The pain becomes more intense, sometimes radiate to the anus, intensify during defecation. Urination is difficult, urine flows with a thin stream. In some cases, urine delay is noted. Subfebrilite or moderate hyperthermia is typical.
- Acute parenchymal. Pronounced general intoxication, hyperthermia up to 38-40 ° C, chills. Dizuric disorders, often an acute delay in urination. Sharp, pulsating pains in the perineum. Difficulty to defecate.
Chronic prostatitis
In rare cases, chronic prostatitis becomes the outcome of an acute process, however, as a rule, a primary chronic course is observed. The temperature occasionally rises to small values. The patient notes weak pain in the perineum, discomfort during the act of urination and defecation. The most characteristic symptom is scarce discharge from the urethra during the act of defecation. The primary chronic form of the disease develops over a significant period of time. She is preceded by stagnation of blood in the capillaries, gradually turning into abacterial prostatitis.
Chronic prostatitis is often a complication of the inflammatory process caused by the causative agent of a specific infection (chlamydia, ureaplasma, gonococcus). Symptoms of a specific inflammatory process in many cases mask the manifestations of the lesion of the prostate. It is possible a slight increase in pain during urination, weak pain in the perineum, scarce discharge from the urethra during defecation. A slight change in the clinical picture often goes unnoticed by the patient.
Chronic inflammation of the prostate gland can be manifested by a burning sensation in the urethra and perineum, dysuria, sexual disorders, increased general fatigue. The consequence of potency violations (or fear of these violations) often becomes mental depression, anxiety and irritability. The clinical picture does not always include all of the listed groups of symptoms, differs in different patients and changes over time. There are three main syndrome characteristic of chronic prostatitis: pain, violations when going to the toilet, sexual disorders.
There are no pain receptors in the prostate fabric. The cause of pain in chronic prostatitis becomes almost inevitable due to abundant innervation of the pelvic organs involvement in the inflammatory process of the nervous paths. Patients complain of pain of various intensity - from weak, aching to intense, violating sleep. There is a change in the nature of pain (enhancement or weakening) with ejaculation, excessive sexual activity or sexual abstinence. Pains radiate to a scrotum, sacrum, crotch, sometimes into the lumbar region.

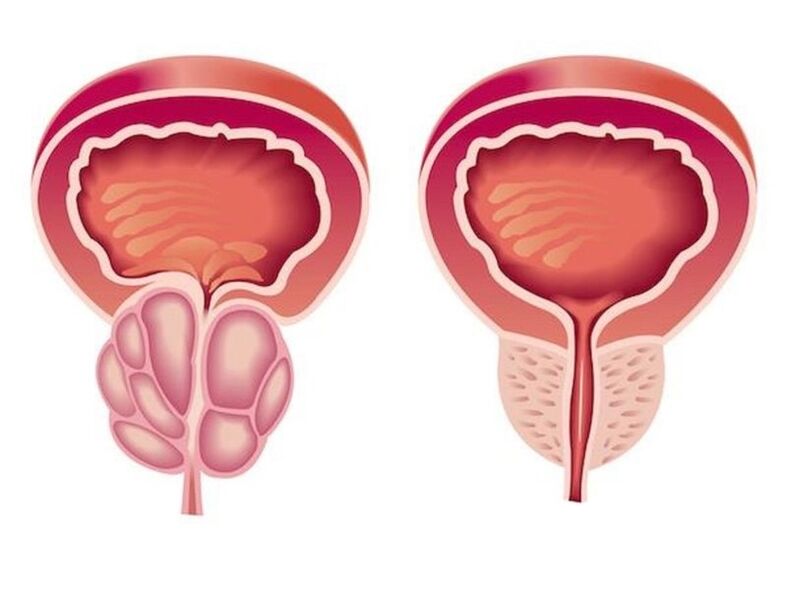
As a result of inflammation in chronic prostatitis, the volume of the prostate squeezing the urethra increases. The lumen of the ureter decreases. The patient has frequent urination, a feeling of incomplete emptying of the bladder. As a rule, dysuric phenomena are expressed in the early stages. Then, compensatory hypertrophy of the muscle layer of the bladder and ureters develops. The symptoms of dysuria during this period are weakening, and then again increased during decompensation of adaptive mechanisms.
In the initial stages, violations in potency may develop, which manifested differently in different patients. Patients may complain of frequent night erections, erased orgasm or deterioration of an erection. Accelerated ejaculation is associated with a decrease in the threshold level of excitation of the center, which is responsible for obtaining an orgasm. Pain for ejaculation can cause a refusal of sexual activity. In the future, sexual disorders become more pronounced. At an advanced stage, impotence develops.
The degree of sexual disorder is determined by many factors, including the sexual constitution and the psychological mood of the patient. Violations of potency and dysuria can be due to both changes in the prostate gland, and how easily the patient can inspire anything. If he has chronic prostatitis, it expects the inevitable development of sexual disorders and urination disorders. Especially often psychogenic disorders in potency and problems with going to the toilet develops in suggestible, alarming patients.
Complications
In the absence of timely treatment of acute prostatitis, there is a significant risk of developing the abscess of the prostate gland. When the purulent focus is formed, the patient’s body temperature rises to 39-40 ° C and can acquire a hectic character. The periods of heat alternate with pronounced chills. Sharp pain in the perineum complicates urination and make defecation impossible.
The growth of edema edema leads to acute urination delay. In rare cases, the abscess spontaneously opens into the urethra or rectum. When opening into the urethra, purulent muddy urine appears with an unpleasant pungent smell, when opening in the rectum, feces contains pus and mucus.
For chronic prostatitis, a wave -like course with periods of prolonged remissions is characteristic, during which inflammation in the prostate proceeds latent or manifests itself in extremely meager symptoms. Patients, whom nothing bothers, often stop treatment, and convert only with the development of complications.
The most frequent complication of the chronic process is the inflammation of the testicles and appendages of the testicles and inflammation of the seed bubbles. The outcome of these diseases often becomes infertility.
Diagnostics

A characteristic clinical picture simplifies the process of diagnosis in acute and chronic prostatitis. Mandatory is made:
- rectal study of the prostate
- The fence of the secretion of the prostate gland to determine the sensitivity of microflora (sowing the secret of the prostate and sowing urine to bacteria).
- An ultrasound of the prostate to identify structural changes (tumors, cysts, adenoma) and differentiation of prostatitis from other diseases is carried out
- A spermogram to exclude or confirm the development of infertility.
Treatment of prostatitis
Treatment of acute prostatitis
Patients with an acute process without complication undergo a course of treatment with an urologist outpatiently. With severe intoxication, suspicion of a purulent process, hospitalization is indicated. Antibacterial therapy is carried out. The drugs are selected taking into account the sensitivity of an infectious agent. Antibiotics are widely used that can penetrate well into prostate tissue (ciprofloxacin, etc. ).
With the development of acute urination delay, against the background of prostatitis, they resort to the installation of a special tube, and not a urethral catheter, because there is a danger of the formation of an abscess of the prostate. With the development of the abscess, an endoscopic transrectal or urethral opening of the abscess is carried out.
Treatment of chronic prostatitis
Treatment of chronic prostatitis should be complex, including etiotropic therapy, physiotherapy, immunity correction:
- Antibiotic therapy. The patient is prescribed long-term antibacterial courses (within 4-8 weeks). The selection of the type and dosage of antibacterial drugs, as well as the determination of the duration of the course of treatment is carried out individually. The drug is chosen based on the sensitivity of microflora based on the results of the sowing of urine and the secret of the prostate.
- Prostate massage. The massage of the gland has a comprehensive effect on the affected organ. During the massage, the inflammatory secret accumulated in the prostate gland is squeezed into the ducts, then enters the urethra and removes from the body. The procedure improves blood circulation in the prostate, which allows minimizing stagnation and provides the best penetration of antibacterial drugs into the tissue of the affected organ.
- Physiotherapy. To improve blood circulation, laser exposure, ultrasonic waves and electromagnetic vibrations are used. If it is impossible to carry out physiotherapeutic procedures, the patient is prescribed warm medicinal microclisms.
In chronic, long -term inflammation, a consultation of an immunologist is indicated for the choice of tactics of immunocorrogative therapy. The patient is given recommendations for a change in lifestyle. The introduction of certain changes to the lifestyle of a patient with chronic prostatitis is both therapeutic and a preventive measure. The patient is recommended to normalize sleep and wakefulness, to establish a diet, and conduct moderate physical activity.

Forecast and prevention
Acute prostatitis is a disease that has a pronounced tendency to chronic. Even with timely adequate treatment, more than half of patients, chronic prostatitis becomes outcome. Recovery is far from always possible, however, with the correct sequential therapy and compliance with the doctor’s recommendations, it is possible to eliminate unpleasant symptoms and achieve a long persistent remission in the chronic process.
Prevention consists in eliminating risk factors. It is necessary to avoid hypothermia, alternate sedentary work and with periods of physical activity, and eat regularly and fully. With constipation, laxatives should be used. One of the preventive measures is the normalization of sexual life, since both excessive sexual activity and sexual abstinence are risk factors in the development of prostatitis. If the symptoms of a urological or sexually transmitted disease appear, you need to consult a doctor in a timely manner.
























